What Changes in Your Tongue May Say About Your Overall Well-Being
For many older adults, the day begins with a series of quiet, rhythmic rituals. You wash your face, perhaps engage in a few gentle stretches to shake off the night’s stiffness, and eventually, you find yourself face-to-face with the bathroom mirror. Most mornings, the reflection is familiar. But occasionally, a subtle shift catches the eye: the tongue, usually a healthy pink, appears shrouded in a mysterious white coating. In the early stages of this discovery, it is easy to dismiss. Common wisdom suggests it’s merely the byproduct of dry winter air, sleeping with one’s mouth open, or perhaps a lingering residue from last night’s dinner. For many, the assumption is that it will simply fade away. In many instances, this optimism is justified; a white tongue is often a benign, fleeting occurrence. However, for those navigating their sixth decade and beyond, these small physical deviations warrant a more sophisticated level of scrutiny. As the body matures, it becomes a more finely tuned instrument—one that is increasingly sensitive to internal imbalances. The tongue, in particular, serves as one of our most responsive biological “dashboards.” Its color, texture, and coating are not random; they are real-time data points reflecting hydration, immune function, medication side effects, and oral hygiene.
The Baseline: What Is “Normal”?
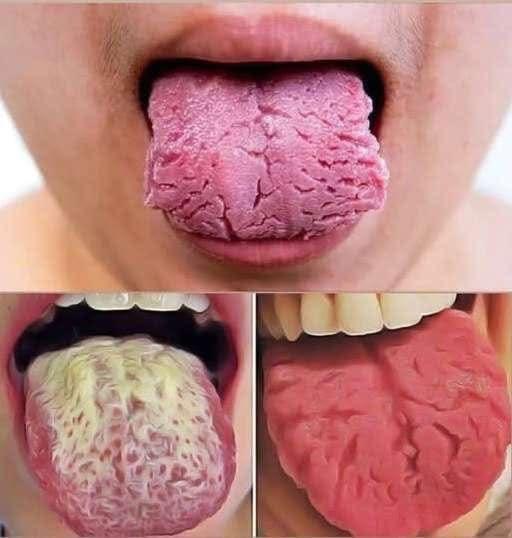
A healthy tongue should be pink, slightly moist, and characterized by an even texture. A very thin, transparent film is perfectly normal—it acts as a protective barrier for the surface. What should raise a red flag is a coating that appears thick, “shaggy,” patchy, or is accompanied by pain.
When the surface becomes pale or heavily blanketed, it is the body’s quiet way of signaling that an adjustment is required. For seniors, understanding these signals is the difference between proactive wellness and reactive medicine.
The Age Factor: Why the Stakes Shift
As we age, the mouth undergoes a quiet transformation. Saliva production—the mouth’s primary self-cleaning mechanism—often begins to wane. The immune system may not respond to minor bacterial imbalances with its former speed, and the introduction of daily maintenance medications can further complicate the oral environment.
Because of these factors, the tongue often acts as a “canary in the coal mine,” showing signs of systemic stress—be it dehydration, nutritional gaps, or minor infections—well before other symptoms manifest. While not every white tongue is an omen of illness, persistence is key. If the coating remains, worsens, or is paired with a “cotton-mouth” sensation or difficulty swallowing, it is time to look deeper.

The Overlooked Culprit: Oral Hygiene Beyond the Teeth
One of the most frequent causes of a coated tongue is a gap in daily maintenance: the tongue itself. While most are diligent about brushing their teeth, the tongue is frequently ignored. This is a tactical error in oral care.
The surface of the tongue is far from smooth; it is a topographical map of thousands of tiny projections called papillae. These structures create microscopic valleys and grooves—prime real estate for food particles, dead skin cells, and bacteria to take up residence.
Over time, this debris forms a visible white biofilm. For older adults, this buildup can accelerate due to several factors:
-
Physical Constraints: Arthritis or reduced hand strength can make thorough brushing a challenge.
-
Sensitive Reflexes: A strong gag reflex often discourages people from cleaning the back of the tongue where buildup is heaviest.
-
Saliva Deficiency: Without adequate saliva to neutralize acids and wash away debris, the tongue loses its natural “rinse cycle.”
The solution is often mechanical. Integrating a tongue scraper or a soft-bristled brush into the morning routine can yield immediate results. For seniors, this isn’t just about aesthetics; a clean mouth directly impacts the ability to taste, the desire to eat, and overall nutritional intake.
Dehydration: The Silent Biological Tax
Perhaps the most powerful, yet silent, contributor to a white tongue in the over-60 demographic is dehydration. As we age, the body’s “thirst center” in the brain becomes less sensitive. Many seniors are functionally dehydrated without ever feeling the urge to drink.
This is often compounded by medications—diuretics for blood pressure, certain heart medications, or bladder control prescriptions—all of which can leaches fluids from the system or dry out the salivary glands. When fluids run low, the mouth becomes a stagnant environment, leading to that tell-tale white, sticky coating.
A white tongue in the morning is often the first sign that your “fluid tank” is running low. Responding to this signal by sipping water consistently throughout the day—regardless of whether you feel thirsty—does more than just clear the tongue; it supports cognitive clarity, joint lubrication, and cardiovascular health.
The Journalist’s Takeaway
The appearance of a white tongue shouldn’t be a source of panic, but it should be a source of curiosity. It is a subtle communication from a body that is working hard to maintain its balance. By paying attention to these small shifts, older adults can manage their health with the quiet confidence that comes from truly knowing how to read the “dashboard” of their own well-being.
In the intricate architecture of the human body, the mouth serves as the gateway to systemic health. For the seasoned adult, however, this gateway often undergoes a series of silent, chemically-driven transformations. When that morning glance in the mirror reveals a persistent white film across the tongue, it is frequently a manifestation of two primary forces: the chemical side effects of modern medicine and the shifting balance of the body’s internal microbiome.
Understanding these shifts is not merely an exercise in vanity; it is a critical component of geriatric wellness. From the drying effects of pharmacological staples to the opportunistic nature of yeast, the “white tongue” of the over-60 demographic is a story of chemistry, immunity, and lifestyle.
The Pharmacological Tax: Dry Mouth and Saliva Flow
Perhaps the most significant contributor to tongue discoloration in seniors is Xerostomia, or chronic dry mouth. This is rarely a natural byproduct of aging itself, but rather a “pharmacological tax” paid for the management of other conditions.
A vast array of essential prescriptions—those managing hypertension, allergies, depression, anxiety, and chronic pain—list reduced saliva flow as a primary side effect. In a moist, healthy environment, saliva acts as a continuous rinse cycle, neutralizing acids and keeping bacterial populations in check. When this flow is stilled, the mouth becomes a stagnant pond where bacteria multiply with impunity. The result is a thick white coating, a persistent unpleasant taste, and a heightened risk for cavities and speech impediments.
Managing this requires a tactical approach:
-
Medical Audit: Consult with a provider to see if medication timing or types can be adjusted.
-
Mechanical Stimulation: Utilize sugar-free lozenges or xylitol-based gums to “prime the pump” of salivary glands.
-
Hydration Routine: Sip water consistently and avoid alcohol-based mouthwashes, which can exacerbate tissue dryness.
Oral Thrush: When the Microbiome Tips
In more acute cases, a white tongue is not merely buildup but a biological overgrowth known as Oral Thrush. This yeast infection (Candida albicans) manifests as creamy, curd-like patches that may migrate to the inner cheeks.
For seniors, the risk of thrush is heightened by several factors:
-
Immune Sensitivity: A naturally maturing immune system may be less adept at keeping yeast populations suppressed.
-
Antibiotic Use: These medications often clear out beneficial bacteria, leaving a vacuum for yeast to fill.
-
Denture Hygiene: Dentures can act as a reservoir for yeast if not sanitized with clinical precision.
Unlike simple debris, thrush can be painful, causing a burning sensation, and may bleed if the surface is disturbed. It is a clear signal that the mouth’s delicate ecological balance has been compromised and often requires professional antifungal intervention.
The Lifestyle Lever: Diet, Habit, and Sleep
While biology and medicine play their parts, daily choices remain a powerful lever for tongue health.
-
The Dietary Footprint: Diets high in refined carbohydrates and sugars provide the exact fuel that bacteria and yeast need to flourish. For seniors who may favor softer, processed foods due to dental sensitivity, this sticky residue can become a permanent fixture on the tongue’s textured surface. Integrating “crunchy” produce like apples or carrots provides a natural mechanical cleaning that helps sweep away film.
-
The Drying Effects of Habits: Smoking and alcohol consumption are double-edged swords; they irritate delicate oral tissues while simultaneously dehydrating the mouth. This creates a cycle of persistent irritation and coating that can only be broken through reduction or cessation.
-
The Sleep Factor: Mouth breathing during sleep—often a result of nasal congestion or sleep apnea—evaporates the “night shift” of saliva production. This results in the heavy “morning tongue” many notice upon waking.
Clinical Red Flags: When to Seek Professional Counsel
While improved hygiene and hydration resolve most cases, a veteran journalist knows that some signs demand an expert’s eye. If a white coating persists for more than three weeks, or if it is accompanied by cracking, swelling, or difficulty swallowing, it is time to exit the “self-care” phase and enter the “clinical” phase.
The tongue is a remarkably honest indicator of internal integrity. It tracks our nutritional status (especially levels of B vitamins and zinc) and our systemic resilience. By observing it with a mixture of curiosity and compassion, we aren’t just looking for a cleaner mouth—we are investing in the long-term dignity and comfort that defines a life well-lived.
In the end, these small signals from the mirror are not cause for alarm, but calls to action. They are reminders that as we age, the body requires a more attentive, intentional partnership. By listening to the quiet wisdom of the body, we ensure that our later chapters are defined by health, social confidence, and a deep-seated physical well-being.